Performing CPR with an Advanced Airway: Key Differences and Techniques
Cardiopulmonary resuscitation (CPR) is a critical life-saving technique used to revive individuals experiencing cardiac arrest. In certain situations, an advanced airway may be inserted to facilitate the delivery of oxygen and improve ventilation. However, performing CPR with an advanced airway requires some adjustments in technique. In this article, we will explore the key differences and techniques involved in performing CPR when an advanced airway is in place.
1. Understanding CPR and Advanced Airway:
CPR and Advanced Airway
Before we delve into the specifics of CPR with an advanced airway, let's briefly understand the basics.
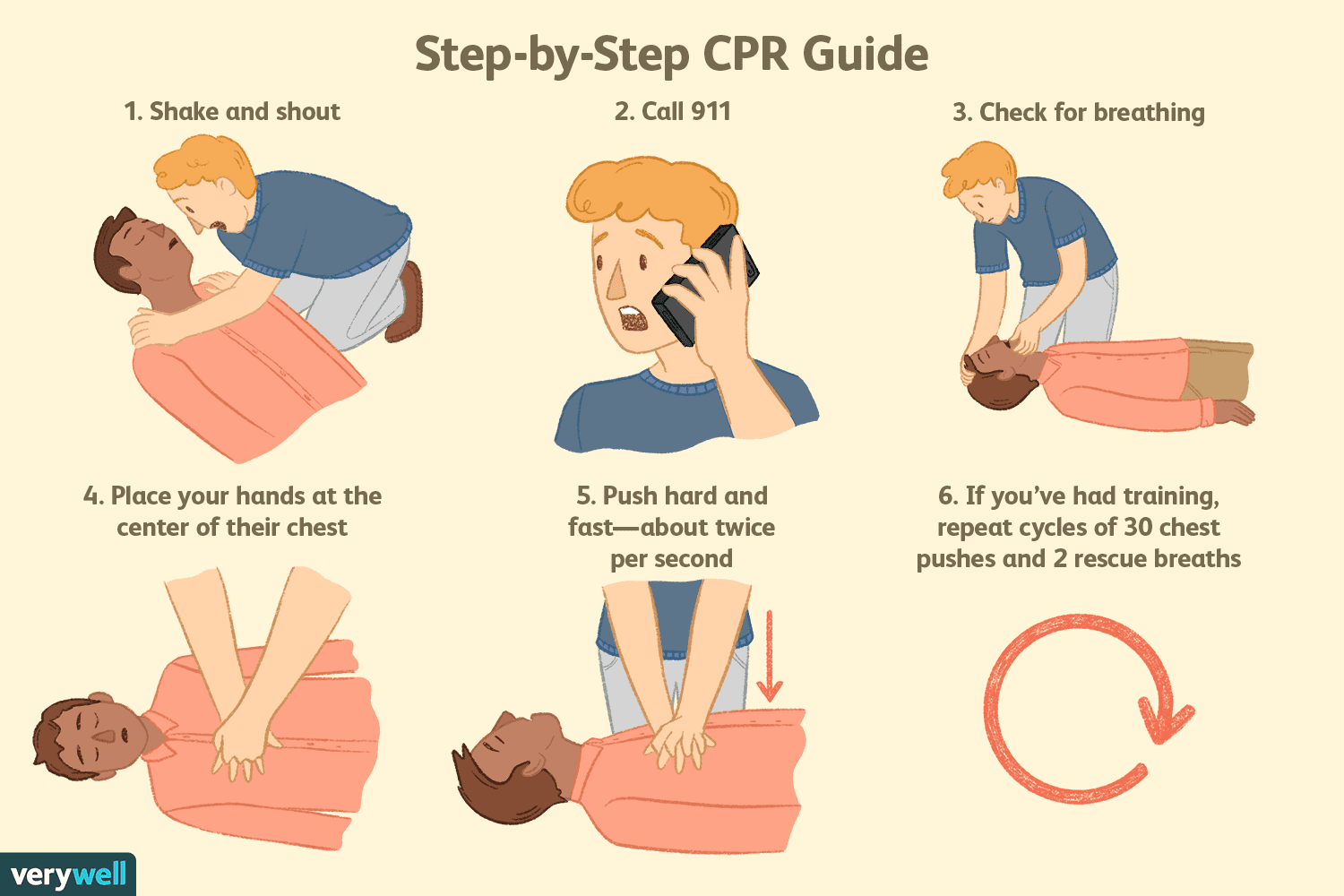
CPR is a combination of chest compressions and rescue breaths performed to maintain blood flow and oxygenation in an individual experiencing cardiac arrest.
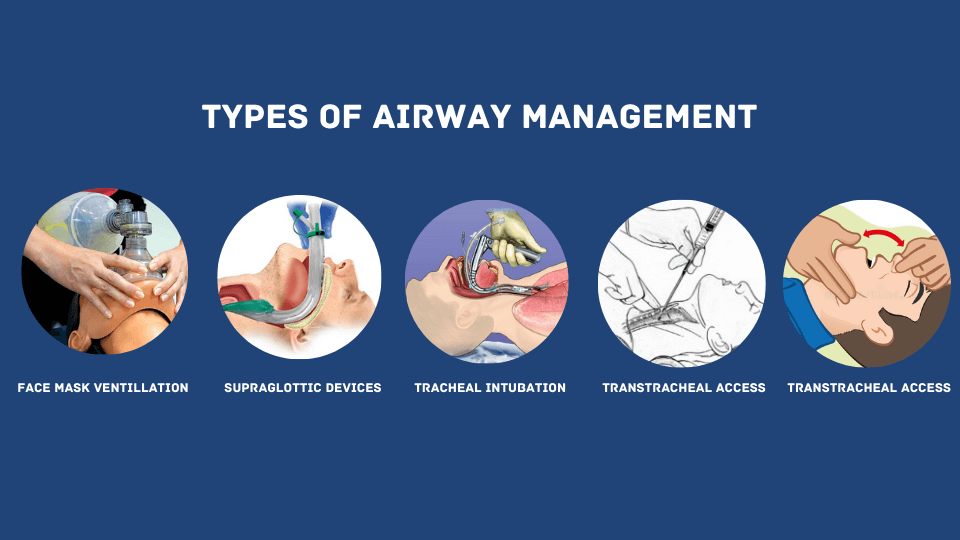
An advanced airway, such as an endotracheal tube or supraglottic airway device, is used to secure the airway and assist with ventilation.
2. The Importance of an Advanced Airway:
When cardiac arrest occurs, maintaining effective ventilation and oxygenation is crucial for the patient's survival.
An advanced airway allows for more controlled and efficient delivery of oxygen, improves the effectiveness of rescue breaths, and reduces interruptions during chest compressions.
3. Key Differences in CPR Technique:
CPR Technique
When an advanced airway is in place, there are several key differences in CPR technique compared to traditional CPR with mouth-to-mouth rescue breaths:
a. Chest Compressions:
Chest compressions remain a vital component of CPR. However, when an advanced airway is in place, chest compressions are uninterrupted and delivered at a rate of 100 to 120 compressions per minute. The rescuer no longer pauses to deliver rescue breaths.
b. Ventilation:
With an advanced airway, the focus shifts primarily to chest compressions rather than ventilation. The rescuer no longer provides mouth-to-mouth rescue breaths but instead focuses on high-quality chest compressions to circulate blood and deliver oxygen.
c. Bag-Valve-Mask (BVM) Ventilation:
When an advanced airway is in place, ventilation is typically provided using a bag-valve-mask device attached to the advanced airway.
Rescuers use the BVM to deliver positive pressure ventilation at a rate of approximately 10 breaths per minute, synchronized with the chest compressions.
d. Compression-to-Ventilation Ratio:
The compression-to-ventilation ratio changes when an advanced airway is in place. It typically becomes continuous chest compressions with a compression-to-ventilation ratio of 30:2, where the rescuer delivers 30 compressions followed by 2 breaths using the BVM.
4. Coordination and Teamwork:
Performing CPR with an advanced airway often requires coordination and teamwork, especially in a clinical or hospital setting.
One rescuer focuses on high-quality chest compressions while another manages ventilation using the bag-valve-mask device.
Effective communication and coordination ensure the delivery of consistent and uninterrupted CPR.
5. Training and Certification:
Given the differences in technique, it is essential for rescuers to receive proper training and certification in performing CPR with an advanced airway.
Healthcare providers, such as doctors, nurses, and paramedics, receive specific training on advanced airway management and the coordination of CPR techniques. Regular recertification and practice are crucial to maintaining competency.
6. Device-Specific Techniques:
Different types of advanced airway devices may require specific techniques for effective ventilation and chest compressions.
For example, with an endotracheal tube, proper positioning and inflation are critical, while supraglottic airway devices require correct placement and seal. Rescuers should receive device-specific training to ensure optimal performance.
7. Monitoring and Adjustments:
During CPR with an advanced airway, continuous monitoring of the patient's response is crucial.
Healthcare providers monitor chest rise, oxygen saturation levels, and end-tidal carbon dioxide (ETCO2) to ensure effective ventilation and chest compressions.
Adjustments may be made as necessary to optimize patient outcomes.
8. Post-CPR Care:
After successful resuscitation, ongoing management and care are necessary for the patient.
This includes monitoring vital signs, administering appropriate medications, and transferring the patient to a higher level of care if needed.
Close observation and support are crucial during the post-CPR phase.
Performing CPR with an advanced airway requires modifications in technique and coordination between rescuers. With an advanced airway in place, chest compressions take precedence over ventilation, and bag-valve-mask devices are used for ventilation. Proper training, certification, and device-specific techniques are essential for effective CPR with an advanced airway. Continuous monitoring and adjustments ensure optimal patient care. By understanding the key differences and techniques involved, healthcare providers can deliver high-quality CPR in critical situations, increasing the chances of survival for individuals in cardiac arrest.